In this week's case discussion from Dr Terry Harvey, this 20x17mm pigmented lesion is present on...

Acquire the knowledge required to safely and confidently diagnose and treat commonly encountered skin lesions.
Skin cancer is one of the most common dermatological conditions seen in general practice – and it is not overly complex to manage if you have the right skill set.
- This course is perfect for practitioners with no to little training in skin cancer.
- Learn various techniques allowing basic treatment of skin cancer cases in the primary care setting.
- This course is for physicians, nurse practitioners, and degree-qualified nurses.
- CPD-accredited and university-assured.
If you have intermediate knowledge in this area, explore the Advanced Certificate of Skin Cancer Medicine. If you have advanced experience in this area, explore Professional Diploma of Skin Cancer Medicine.
Fulfils 50 hrs for medical professionals in Australia*
100% online
Online + workshop
Fully online: $1595
Online + workshop: from $2395
Special rates available
70.5 hrs
Self-paced
2024
25 May in Melbourne
15 Jun in Adelaide
24 Aug in Brisbane
21 Sep in Sydney
12 Oct in Melbourne
9 Nov in Perth
*provided an outcome measurement activity with a minimum of 5 hours is completed.

- Diagnose benign and malignant lesions with dermoscopy.
- Manage skin cancer cases in-house and reduce referrals.
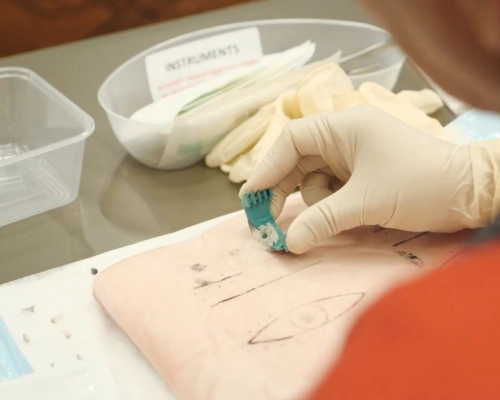
- Perform punch and shave biopsies, elliptical excisions, suturing, and topical treatments for various skin cancers.
- Increase clinic revenue by adding skin cancer checks and treatments to your practice.
- Streamline billing and workflow using Medicare guidelines and best practices.
Get unlimited access to all course content, additional learning materials, ongoing post-course support, and more.
*These topics are covered during the hands-on practical sessions in the optional skills workshop. View the workshop program.
This course focuses on the foundations relating to skin cancer medicine. Participants will acquire the knowledge required to safely and confidently diagnose and treat commonly encountered skin lesions. It is the ideal starting point to build core knowledge in skin cancer management and acquire vital diagnostic skills and basic management techniques to provide effective care to patients.
Unit one introduces the foundation information required for skin cancer medicine and outlines the content of the course. Unit two describes the BEST protocol (BEnign or Suspicious Test) and divides lesions into benign or suspicious with guidelines and clinical images of pigmented skin lesions. Benign lesions require no action and suspicious lesions require biopsy or referral. A quiz with clinical and dermoscopic images to select benign or suspicious lesions is provided, with contextual answers as part of this unit.
Unit three discusses the importance of skin checks and commences with a table dividing assessment of skin cancer risk into three categories: high, medium and low risk and includes patient self-examination and opportunistic skin check. The unit describes how to perform a skin examination and includes lesion history, general medical history, allergies and current medications. The unit includes a video of a systemic total skin examination. Unit four describes partial and complete punch and shave biopsy techniques. The unit concludes with a patient case showing cylindrical portion of skin bearing a dark pigmented surface for which biopsy is recommended. The pathology report is provided as the lesion was partially excised and sent for examination.
This course focuses on the approach to pigmented skin lesions relating to skin cancer medicine. Participants will acquire the knowledge required to safely and confidently diagnose and treat commonly encountered skin lesions. It is the ideal starting point to build core knowledge in skin cancer management and acquire vital diagnostic skills and basic management techniques to provide effective care to patients.
Unit one discusses common benign lesions including freckles, solar lentigo, seborrheic keratosis, haemangioma, dermatofibroma and blue nevi. Normal and dermoscopic clinical images are provided to demonstrate patterns and assists with analysis. Benign lesions can mimic skin cancers and careful examination is required to decide management steps. The signs of common benign lesions that may be skin cancer are discussed in detail. A medico-legal case is included for a patient where a melanoma was masquerading as a benign lesion.
Unit two begins with the description of dermoscopy including examples of dermoscopic devices used for this technique. The 3-point checklist consists of asymmetry in colour or structures, atypical network and blue-white structures (white scar-like depigmentation or blue pepper-like, globular or structure-less areas), showing various clinical dermoscopic images of lesions.
This unit covers dysplastic nevi and melanoma. A table is shown of the relationship between nevus, dysplastic nevus and melanoma and includes a table of relative risk factors for melanoma. Several types of melanomas and treatment options are listed and supported by clinical images. The unit concludes with key points for detecting benign or suspicious lesions.
This course focuses on the approach to non-pigmented skin lesions relating to skin cancer medicine. Participants will acquire the knowledge required to safely and confidently diagnose and treat commonly encountered skin lesions. It is the ideal starting point to build core knowledge in skin cancer management and acquire vital diagnostic skills and basic management techniques to provide effective care to patients.
This unit starts with a clinical description of solar keratosis and outlines treatment options including field treatment. Attention is also paid to Bowen’s disease (a very early form of skin cancer), including symptoms, diagnosis (punch biopsy) and treatment. Dermoscopic images of both conditions are provided.
This unit describes keratocanthoma, a low-grade malignancy that requires a deep incision biopsy, and also discusses squamous cell carcinoma, a common cancer due to chronic, cumulative, sun exposure. Treatment options include surgery, curettage and cautery, referral or radiation therapy. Clinical images of both conditions are provided.
Unit three describes basal cell carcinoma, the most common human cancer due to intermittent excessive sun exposure. BCC can be classified as non-aggressive (superficial, nodular) or aggressive (sclerosing/infiltrating/ micronodular/multifocal/solid). Clinical images of the different types of basal cell carcinoma, diagnosis and treatment options are included.
This course focuses on dermatopathology relating to skin cancer medicine. Participants will learn about the best approach to pathology requests and how to interpret pathology reports. This unit lists the steps that occur when a skin sample is sent for pathology testing. The course then continues with images of pathology processing of a punch, shave and excision biopsy. The report interpretation is discussed including interobserver agreement, clues to pathologist uncertainty, reconciliation of unexpected results, assessment of margins and errors that occur in dermatopathology.
This course focuses on topical treatments options and medico-legal issues relating to skin cancer medicine. Participants will learn about the topical treatments, the (contra-)indications and dose of Imiquimod 5% cream used for treating superficial basal cell carcinomas, and 5-fluorouracil (5-FU) 5% cream used for preventing and treating SCC and Bowen’s disease. A table of topical treatment regimens in primary care for solar keratosis is provided. An extensive list of tips including cost, pre-treatment and patient-education is provided. The unit looks at different treatment options for solar keratosis. Clinical images of lesions at the initial visit, during and after topical treatment are shown.
Medico-legal tips and resources are listed in unit two. The importance of detailed medical record keeping, follow up and recall systems and patient consent are included. The unit concludes with a medico-legal case of a middle-aged man with a past medical history of non-melanoma skin cancer, the resulting investigation and the problems in how the case was managed that resulted in medico-legal action.
This course focuses on preparation for surgical treatment relating to skin cancer medicine. Participants will learn the fundamental principles when preparing for and performing skin cancer surgery. The fundamentals include an aseptic approach using sterile equipment, sutures and dressings and emphasizes the importance of clean skin, operator preparation and environment. The unit then looks at local anaesthetics and haemostasis. Equipment for wound closure and sutures are listed including the fundamentals of closing the defect. Recommended suture removal times and the suture techniques, use of prophylactic antibiotics and anticoagulants conclude this unit.
Unit two describes the punch and shave biopsy and includes video and clinical images of these procedures.
This course focuses on excision and repair relating to skin cancer medicine. Participants will learn the instruments used for wound closure and sutures used for skin closure, including suture technique and removal times. Drawings and description of the simple interrupted suture are discussed, including a recording of this procedure.
Unit two emphasizes the importance of using an absorbable suture and shows drawings of a conventional buried dermal suture. The unit concludes with a recording of this procedure.
Unit three focuses on the preparation for an elliptical excision, including placement of excisions for the best cosmetic result. It outlines the steps leading to performing the ellipse including surgical marking up. The procedure is described and illustrated by drawings of the incision considering maximal skin tension lines and fusiform excision lines. The unit concludes with a video of this procedure.
This course focuses on medicare billing relating to skin cancer medicine. Participants will learn about the list of billings items and a quick reference card of skin cancer item number guide is discussed.
Unit two details what is included in each applicable procedural item number and describes the multiple services rules as well as bulk billed fee for a procedure. Billing of punch and shave biopsy are explained as well as non-surgical procedures including cryotherapy (benign or pre-malignant), serial curettage and lesion removal, considering site, size and type. The unit concludes with billing of post operative care and treatment after a procedure.
If you're not interested in pursuing a full certificate in this field but simply want to enhance your skills in specific topics covered in this course, you can access the content of this and other courses for a flat fee of $83 per month (paid annually) within HealthCert 365.

Chief Medical Officer,
National Skin Cancer Centres
Professor David Wilkinson is a registered general practitioner and public health medicine expert. Prior to taking up the role as Chief Medical Officer with National Skin Cancer Centres, he was Deputy Vice-Chancellor of the Macquarie University, Sydney for eight years, and before that was Dean of Medicine at The University of Queensland for nine years.
Since 2004, David’s clinical work has focused on skin cancer medicine in primary care. He has published research papers on the topic, designed and led development of the only Master of Medicine degree in skin cancer, and helped develop and present a suite of skin cancer short courses delivered by HealthCert. He has taught almost 7,000 GPs the basics of skin cancer medicine in primary care.

Dr Simon Clark runs the pathology component of the postgraduate certificate courses in skin cancer medicine at The University of Queensland and lectures in the Masters of Medicine course. He has been involved in dermatopathology education for more than 20 years, training registrars in dermatology, pathology and plastic surgery. More recently he has been active in GP education. One of the best known dermatopathologists in Australia, Simon was recently appointed a visiting professor in dermatology at the Tehran University of Medical Sciences.

Paul Elmslie has over 20 years' work experience with a focus on skin cancer. An early pioneer in the development of skin cancer clinics, Paul operates Australia's leading network of dedicated skin cancer facilities and continues to lead the industry through HealthCert Education, the world's first integrated university-assured education provider for medical professionals. Paul has authored books and speaks at conferences all over the world. He has completed business programs with Harvard, MIT and London School of Business, and holds an MBA.

Born and educated in Adelaide, a true entrepreneur, Matt Woollard has run various businesses in the areas of advertising, entertainment and retail.
Matt began his career in skin cancer in 2000 as the second employee of Skin Alert. He worked alongside Paul Elmslie to grow the company to 14 skin cancer clinics throughout Australia in seven years.
Matt has worked as a consultant in education with companies like HealthCert, Notre Dame Australia, University of Melbourne, The University of Queensland, Zimmer, NSW Health and the RACGP.
Matt is now the Chief Operations Officer of National Skin Cancer Centres (NSCC). Established in 2016, NSCC builds and operates skin cancer clinics across Australia, starting out with just one centre and now expanding to eight, with another 22 scheduled to join the group.
Matt’s area of expertise in the industry is operations, based on a very strong understanding of skin cancer medicine including all aspects of Medicare in primary care.

Study at your own pace and to your own schedule.

Complete your course online and receive all the benefits of online study, then put theory into practice at a small-group workshop.

Easily meet your CPD requirements and gain valuable skills – all in one place for $83 per month.
from $1595
*provided an outcome measurement activity with a minimum of 5 hours is completed.
Bundle two courses and save 5%, or three courses and save 10% upon enrolment.
Talk to us about deferred payment options, registrar scholarships and special rates.


Great course! it is very relevant to all practising GPs. Who knew that there is a pathologist "secret". Every GP should know this!
Dr M. Parashar
Highly satisfied. Real patients and cases enhance the learning experience. I will attend the advanced course.
Dr N. Kazi
Don't miss this course! It's interesting, practical and enjoyable. After attending courses for 30 years, I rank this as number one. The course is very useful to all doctors who diagnose and treat skin lesions. Top marks to the organisers.
Dr P. Laundy
Everything was very relevant and easy to understand. Certainly in a very different league to all the other courses I have attended.
Dr M. Kaur
I wish I had completed this course two years ago. My time in general practice so far has not enhanced my diagnostic or surgical skills and I have been scared about skin checks! I actually feel not only confident but empowered. A fantastic course! Thank you!
Dr A. Mooney
| RACGP Activity Number | ACRRM Activity Number | Activity Title | Education Hours | Performance Hours | Outcome Hours | Total Hours | ||
|---|---|---|---|---|---|---|---|---|
| 401610 | 27990 | Dermatopathology | 401610 | 27990 | 4 | 5 | 0 | 9 |
| 401623 | 27993 | Medicare billing | 401623 | 27993 | 3.5 | 5 | 0 | 8.5 |
| 401495 | 27986 | The foundations | 401495 | 27986 | 4 | 5 | 0 | 9 |
| 401616 | 28001 | Topical treatment and medico-legal issues | 401616 | 28001 | 4 | 5 | 0 | 9 |
| 401566 | 27987 | An approach to pigmented skin lesions | 401566 | 27987 | 4 | 5 | 0 | 9 |
| 401621 | 28031 | Excision and repair | 401621 | 28031 | 3.5 | 5 | 0 | 8.5 |
| 401618 | 28029 | Preparation for surgical treatment | 401618 | 28029 | 3.5 | 5 | 0 | 8.5 |
| 401605 | 27989 | An approach non-pigmented skin lesions | 401605 | 27989 | 4 | 5 | 0 | 9 |
| 800366 | 32970 | Topical Treatments Outcome Improvement Activity | 800366 | 32970 | 0 | 0 | 8.5 | 8.5 |
| Grand Total | 79 | |||||||
Outcome measurement activities are not a requirement of our professional and advanced certificates. You may use an optional HealthCert outcome measurement activity or develop your own.
HealthCert provides several options to meet your outcome measurement hours requirement. These options are self-submitted activities and hours may vary depending on your focus area.
The purpose of outcome measurement activities is to improve your clinical confidence in managing an identified learning gap. The outcome improvement activities are designed to examine current clinical care, align clinical practice with best practice standards and identify opportunities for improvement.
The Professional Certificate of Skin Cancer Medicine is the ideal starting point for medical professionals who wish to build your core knowledge in skin cancer management and acquire vital diagnostic skills and basic management techniques to provide effective care to patients with skin cancer concerns. Participants will learn proven techniques to independently and confidently diagnose and treat skin lesions in primary care.
This course is for physicians, nurse practitioners, and degree-qualified nurses. It assumes no prior knowledge or training in the field, although HealthCert recommends that participants have some exposure to skin cancer management before enrolling in this course.
Participants do not have to pass an IELTS test but, as the courses are delivered in English, proficiency in listening, reading and writing in English is assumed.
Participants will require access to a computer/laptop, an internet connection and a basic level of technology proficiency to access and navigate the online learning portal.
Professionally accredited qualifications and prior studies may be recognised for entry into this course. Please send an email to credit@healthcert.com for an individual assessment of your prior qualifications and experience.
This email should contain information about your educational history and work experience that specifically pertain to the content and procedures covered in the course.
Please include any applicable certificates and course outlines from previous education. The relevant Course Chair will make a determination on your application within two to three weeks.
This certificate course meets the minimum 50 hours CPD annual requirement across all three mandatory CPD activity types, provided an outcome measurement activity with a minimum of five hours is completed. You may use an optional HealthCert outcome measurement activity or develop your own.
Outcome measurement activities are not a requirement of Professional or Advanced Certificates.
Upon successful completion of the course requirements, course participants will receive the Professional Certificate
This certificate course:
To learn more about the delivery of certificates in Australia and overseas, please visit our FAQs.
Professional Diploma Pathway
This course is the first stage of the three-part professional diploma pathway. The full pathway is Professional Certificate of Skin Cancer Medicine, Advanced Certificate of Skin Cancer Medicine and Professional Diploma of Skin Cancer Medicine.
RPL with The University of Queensland
The Professional Diploma of Skin Cancer Medicine is guaranteed for RPL for the unit IMED7010, part of the Graduate Certificate of Medicine (Skin Cancer) which is the first step in the Master of Medicine (Skin Cancer) at The University of Queensland. There are no further requirements for this RPL, it is automatic and guaranteed and provides a saving on fees. View The University of Queensland, Master of Medicine (Skin Cancer) program.
RPL with Torrens University
This postgraduate pathway is for General Practitioners and degree-qualified medical practitioners who have successfully completed a HealthCert Professional Diploma (all three levels) in Skin Cancer Medicine, Skin Cancer Surgery or Dermoscopy. The following postgraduate course is offered entirely online through Torrens University: Master of Business Administration (MBA). Recognition of Prior Learning (RPL) is available for two general electives for any HealthCert Professional Diploma. In cases where a HealthCert alumni has completed two Professional Diplomas, they will be able to apply for four general electives towards the MBA. This will be helpful to further develop business, management and leadership capabilities. Please apply directly to Torrens University.
Postgraduate Diploma in Dermatology with the University of Plymouth
The Postgraduate Diploma in Dermatology is studied through the Rila Institute of Health Sciences and awarded by the University of Plymouth (UK).
There are three modules in the Postgraduate Diploma. Medical professionals who successfully complete the HealthCert Professional Certificate of Skin Cancer Medicine, Advanced Certificate of Skin Cancer
The Postgraduate Diploma is mainly delivered online. No practical workshops will be required due to the APCL from the HealthCert qualifications. Overall there will be a time saving of 40 per cent of the postgraduate program due to the APCL. Exams will be held in Perth, Western Australia.
When the Postgraduate Diploma has been successfully completed, medical professionals can apply for credit from the Postgraduate Diploma to the Master of Science in the specialism awarded by the University of Plymouth.
Certified Clinical Attachments Pathway
Doctors participating the Skin Cancer Medicine program can attend a HealthCert Clinical Attachment at a clinic or university teaching hospital to further refine and enhance their professional knowledge. A HealthCert Australian Clinical Attachment is recommended as the first clinical attachment and a HealthCert International Clinical Attachment is recommended for subsequent clinical attachments.
This organisation is an RACGP-accredited CPD provider under the RACGP CPD Program.








Don't see your question? Explore other faqs or talk to us.
Fees will vary based on the program and study option selected (fully online vs online + optional practical workshop). Payments can be made upfront or in monthly instalments. Special rates and various payment options are available. GP registrars and doctors in training enjoy a scholarship of up to $500. Talk to us to learn more.
Completion of any HealthCert course or attendance at an event will enable you to access the HealthCert Alumni Program which includes:
HealthCert Education is pleased to issue digital credentials for alumni. Digital credentials are a permanent online record of your successful completion of a HealthCert course and are issued to all course participants in addition to PDF certificates. If you are based in Australia, you also have the option to order a hard copy of your digital certificate for a small additional fee.
The recommended study duration of this certificate course is 70.5 hours, which includes study of the pre-course activities and readings, online lectures, live tutorials, and online assessment. This self-paced course offers the flexibility of 100% online study in your own time, at your own pace, in your own home or office, with no mandatory face-to-face requirements. You are not required to be online at specific times but can view and replay video lectures at your convenience.
All HealthCert courses meet World Federation of Medical Education standards. This certificate course qualifies for CPD hours from the Royal Australian College of General Practitioners (RACGP) and the Australian College of Rural and Remote Medicine (ACRRM) in Australia. It is recognised by the Royal New Zealand College of General Practitioners (RNZCGP) in New Zealand. It is recognised by the Hong Kong College of Family Physicians (HKCFP) in China. It is a self-submitted activity in Dubai and the United Kingdom. It is a self-submitted activity through the College of Family Physicians in Canada. If you live or work outside one of the above-mentioned countries, please contact us on admin@healthcert.com to discuss whether this course can be recognised in your country.
Want to stay up-to-date with the latest case studies, podcasts, free video tutorials and medical research articles pertinent to primary care?
Our Education Advisors can assist you with any queries and tailor our education pathway to suit your current expertise, interests and career goals.